The Amsler grid represents one of ophthalmology’s most elegant yet powerful diagnostic tools, serving as a sentinel for macular health and central vision integrity. This simple 10-centimetre square grid, adorned with a central fixation dot, has revolutionised how eye care professionals and patients monitor for subtle changes in central visual function. When distortions appear in the grid’s seemingly straightforward pattern of intersecting lines, they often herald the presence of serious retinal conditions that demand immediate attention.
Understanding the clinical significance of Amsler grid distortions extends far beyond recognising wavy lines or missing squares. These visual aberrations, known medically as metamorphopsia , provide crucial insights into the structural integrity of the macula—the retina’s central region responsible for sharp, detailed vision. For the millions of individuals at risk of age-related macular degeneration and other retinal pathologies, regular Amsler grid testing serves as an early warning system that can mean the difference between preserved sight and irreversible vision loss.
Amsler grid test methodology and diagnostic applications
The systematic approach to Amsler grid testing requires precise methodology to ensure reliable results and meaningful clinical interpretation. Marc Amsler, the Swiss ophthalmologist who developed this assessment tool, created seven distinct variations of the grid test, though the standard Chart 1 remains the most widely utilised in clinical practice and home monitoring protocols.
Standard 10-centimetre grid configuration and visual angle measurements
The traditional Amsler grid measures exactly 10 centimetres by 10 centimetres, divided into 400 individual squares arranged in a 20×20 configuration. When held at the standard testing distance of 30 centimetres (approximately 12 inches), each square subtends a visual angle of one degree, creating a total testing field of 20 degrees. This specific angular measurement proves critical for detecting central visual field defects that might otherwise escape notice during routine activities.
The grid’s black lines on white background (or white lines on black background in certain variations) create sufficient contrast to reveal subtle distortions in macular function. The central fixation dot serves as an anchor point, ensuring that the foveal region—the macula’s most sensitive area—remains consistently positioned during testing. This standardised configuration allows for reproducible results across different testing sessions and enables clinicians to track disease progression over time.
Monocular testing protocols for macular function assessment
Effective Amsler grid testing mandates monocular evaluation , meaning each eye must be tested individually while the other remains completely covered. This protocol prevents the phenomenon of binocular summation, where a healthy eye compensates for deficits in its affected counterpart, potentially masking significant pathology. Patients often express surprise when unilateral macular disease becomes apparent only during monocular testing, having experienced no noticeable symptoms during normal binocular viewing.
The testing procedure requires patients to maintain steady fixation on the central dot while using peripheral awareness to evaluate the grid’s integrity. Any perception of wavy lines, missing segments, blurred areas, or distorted squares warrants immediate professional evaluation. The critical nature of this testing protocol cannot be overstated—delays in recognising new distortions can result in irreversible vision loss, particularly in cases of wet age-related macular degeneration.
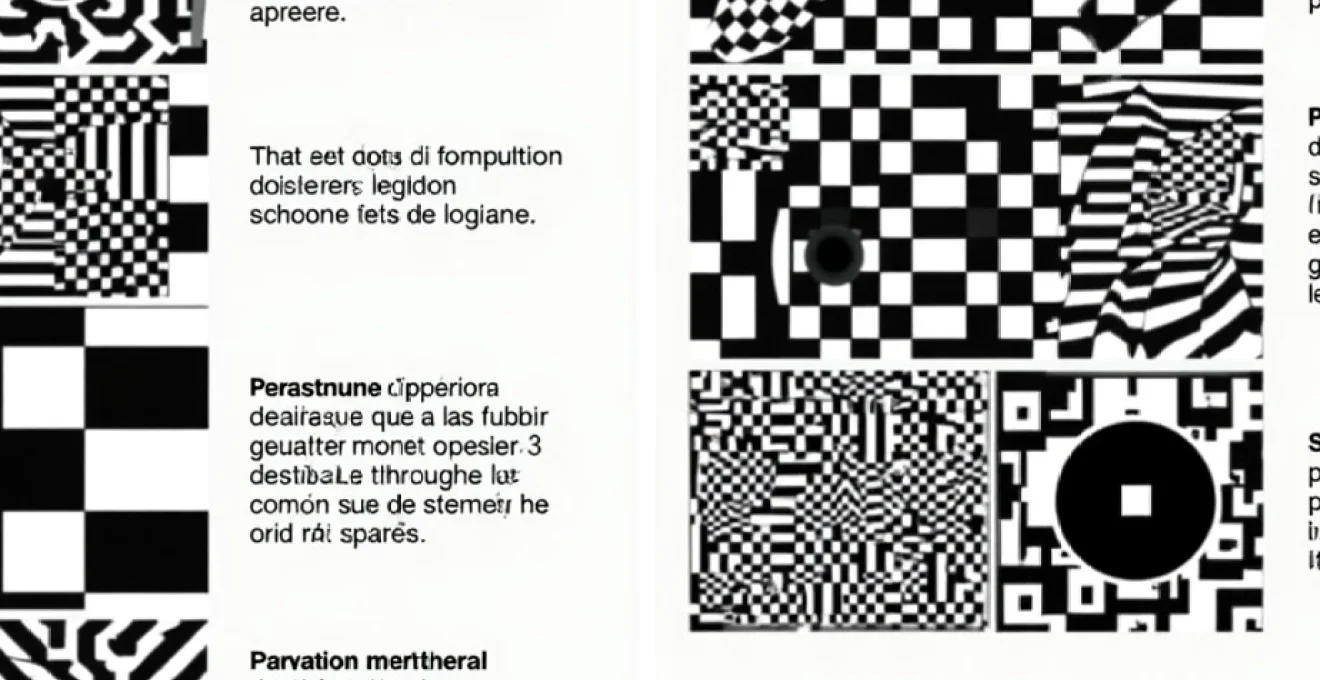
White-on-black versus Black-on-White grid variations
Amsler’s original seven chart variations include both positive contrast (black lines on white background) and negative contrast (white lines on black background) configurations. Research indicates that certain retinal pathologies demonstrate enhanced detectability with specific contrast presentations. White-on-black grids may prove superior for detecting subtle scotomas in conditions such as central serous chorioretinopathy, while traditional black-on-white grids remain optimal for most macular degeneration monitoring.
The choice between contrast variations often depends on individual patient characteristics and specific clinical indications. Patients with advanced cataracts or significant media opacities may benefit from the enhanced contrast provided by white-on-black configurations. Additionally, some individuals with early macular changes report improved distortion detection using negative contrast grids, though this varies considerably among patients.
Digital amsler grid applications and smartphone integration
Modern technology has transformed traditional paper-based Amsler grid testing through sophisticated smartphone applications and tablet-based platforms. These digital solutions offer several advantages, including consistent screen illumination, standardised grid dimensions, and automated testing reminders. However, the critical importance of proper calibration cannot be overlooked—screen size, viewing distance, and brightness settings must align with established testing protocols to ensure clinical validity.
Digital Amsler grid applications often incorporate additional features such as distortion mapping, where patients can mark specific areas of visual abnormality directly on the screen. This capability provides valuable documentation for healthcare providers and enables more precise monitoring of disease progression. Nevertheless, digital testing should complement rather than replace regular professional eye examinations, as comprehensive macular evaluation requires sophisticated imaging and clinical expertise.
Macular pathology detection through grid distortion patterns
Different retinal conditions produce characteristic distortion patterns on Amsler grid testing, creating distinctive signatures that experienced clinicians can recognise and interpret. Understanding these pathognomonic findings enables both healthcare professionals and patients to appreciate the clinical significance of specific visual changes and respond appropriately to concerning symptoms.
Age-related macular degeneration metamorphopsia characteristics
Age-related macular degeneration (AMD) represents the leading cause of severe vision loss in individuals over 65, affecting approximately 600,000 people in the United Kingdom alone. The condition manifests through two distinct forms: dry AMD, characterised by drusen formation and geographic atrophy, and wet AMD, featuring choroidal neovascularisation and fluid accumulation. Each form produces specific Amsler grid abnormalities that reflect underlying pathophysiology.
Dry AMD typically presents with subtle grid distortions, including mild waviness of lines and small areas of decreased visual sensitivity. These changes often develop gradually over months or years, making regular monitoring essential for detecting progression. In contrast, wet AMD can produce dramatic grid alterations within days or weeks. Patients frequently report severe line distortion, central blind spots, and areas where grid squares appear completely missing or darkened.
The metamorphopsia associated with wet AMD results from subretinal or intraretinal fluid accumulation, which physically displaces photoreceptors and disrupts normal visual processing. Straight lines may appear severely curved, resembling waves or hills, while affected areas often exhibit reduced brightness or complete scotomas. The rapid onset of these symptoms necessitates emergency ophthalmological evaluation, as prompt treatment with anti-VEGF injections can preserve remaining vision and prevent further deterioration.
Central serous chorioretinopathy distortion signatures
Central serous chorioretinopathy (CSC) produces distinctive Amsler grid abnormalities that reflect its unique pathophysiology involving serous retinal detachment. Patients typically experience a well-defined central or paracentral scotoma, often described as a dark or grey spot that obscures portions of the grid. The surrounding area frequently demonstrates metamorphopsia, with straight lines appearing curved or bent around the edges of the affected region.
The distortions associated with CSC often fluctuate in severity, corresponding to variations in subretinal fluid levels. Some patients report that grid abnormalities appear more pronounced under certain lighting conditions or times of day. This variability can complicate diagnosis and monitoring, emphasising the importance of consistent testing protocols and professional evaluation when symptoms arise.
Epiretinal membrane contraction effects on grid perception
Epiretinal membranes, also known as macular puckers or cellophane maculopathy, create characteristic grid distortions that reflect mechanical retinal distortion rather than fluid accumulation. The fibrous tissue growth on the retinal surface contracts over time, causing physical wrinkling and displacement of underlying photoreceptors. This mechanical distortion produces specific Amsler grid abnormalities that differ markedly from fluid-related pathologies.
Patients with epiretinal membranes typically report that grid lines appear stretched, twisted, or compressed in the affected area. The distortions often have a directional quality, following the orientation of membrane contraction. Unlike the fluctuating symptoms seen in CSC, epiretinal membrane distortions tend to remain stable or progress gradually over extended periods, reflecting the slow nature of fibrous tissue contraction.
Macular hole progressive distortion manifestations
Full-thickness macular holes produce pathognomonic Amsler grid findings that evolve through distinct stages of hole formation and enlargement. Initially, patients may notice a small grey or dark spot overlying the central fixation dot, representing the earliest stage of foveal tissue loss. As the hole enlarges, the central scotoma expands, and surrounding areas often exhibit metamorphopsia due to associated retinal elevation and distortion.
The progressive nature of macular hole formation means that Amsler grid abnormalities typically worsen over time without surgical intervention. Early-stage holes may produce subtle central dimming or small scotomas that patients might initially dismiss as insignificant. However, prompt recognition and treatment of these early changes through vitrectomy surgery can restore significant visual function and prevent further deterioration.
Diabetic macular oedema grid abnormalities
Diabetic macular oedema creates complex Amsler grid distortions that reflect the multifocal nature of diabetic retinal damage. Unlike conditions that typically affect a single, well-defined area, diabetic oedema often produces scattered abnormalities across the central visual field. Patients may report multiple small areas of distortion, intermittent line waviness, and regions of decreased grid visibility.
The dynamic nature of diabetic macular oedema means that grid abnormalities can fluctuate significantly based on glycaemic control, blood pressure management, and other systemic factors. Some patients notice that distortions appear more prominent during periods of poor diabetes control or after meals with high glucose loads. This variability underscores the importance of comprehensive diabetes management in preserving retinal health and visual function.
The rapid detection of new Amsler grid distortions can mean the difference between treatable disease and irreversible vision loss, particularly in cases of wet age-related macular degeneration where treatment delays of even days can significantly impact visual outcomes.
Neurological scotoma identification using amsler testing
While Amsler grid testing primarily focuses on macular pathology detection, it also serves as a valuable screening tool for neurological conditions affecting the visual pathway. Central and paracentral scotomas resulting from optic nerve disease, chiasmal compression, or cortical lesions can produce characteristic grid abnormalities that warrant further neurological investigation.
Central scotoma mapping in stargardt disease
Stargardt disease, the most common inherited macular dystrophy, typically presents with progressive central vision loss that manifests clearly on Amsler grid testing. Unlike age-related conditions, Stargardt disease often affects younger individuals, making early detection through systematic grid testing particularly valuable for genetic counselling and family screening purposes.
The central scotomas associated with Stargardt disease tend to be well-defined and symmetric, reflecting the bilateral nature of this genetic condition. Patients often report that the central fixation dot appears dim or completely absent, while surrounding grid areas may show varying degrees of distortion. The progressive nature of photoreceptor degeneration in Stargardt disease means that scotomas typically enlarge over time, making regular monitoring essential for tracking disease progression.
Paracentral scotoma detection in glaucomatous optic neuropathy
While glaucoma primarily affects peripheral vision, certain forms of the disease can produce paracentral scotomas detectable through Amsler grid testing. These defects typically appear as small, well-defined areas where grid lines disappear or become significantly dimmed. The location of these scotomas often corresponds to specific retinal nerve fibre bundle defects, providing valuable information about disease severity and progression.
Normal-tension glaucoma and certain forms of primary open-angle glaucoma may present with central visual field involvement earlier than traditionally recognised. Amsler grid abnormalities in these cases often precede detectable changes on standard automated perimetry, highlighting the grid’s value as a sensitive screening tool for early glaucomatous damage.
Temporal visual field defects in chiasmal compression
Lesions affecting the optic chiasm, such as pituitary adenomas or craniopharyngiomas, can produce temporal visual field defects that extend into the central visual field tested by the Amsler grid. These neurological conditions typically create bilateral temporal hemianopsias, where the temporal portion of each eye’s visual field becomes affected.
On Amsler grid testing, chiasmal compression may manifest as consistent absence or dimming of grid lines in the temporal portion of the central visual field. Unlike retinal pathology, these defects typically respect the vertical meridian and appear similar in both eyes when tested monocularly. The recognition of such patterns should prompt immediate neurological evaluation and brain imaging studies.
Homonymous hemianopia patterns in stroke patients
Cerebral infarctions affecting the visual cortex or optic radiations can produce homonymous hemianopsias that extend into the central visual field. These neurological defects appear as consistent loss of vision in the same portion of the visual field in both eyes, creating characteristic Amsler grid abnormalities that differ markedly from retinal pathology.
Stroke-related visual field defects often have sharp borders and complete loss of vision within affected areas, unlike the gradual transitions typically seen in retinal disease. Patients may report that entire sections of the Amsler grid appear completely absent or that they lose awareness of grid portions during testing. These findings, particularly when they occur suddenly, require emergency neurological evaluation.
Amsler grid limitations and False-Negative results
Despite its clinical utility and widespread adoption, the Amsler grid possesses inherent limitations that clinicians and patients must understand to ensure appropriate interpretation and clinical decision-making. Research indicates that the traditional Amsler grid may miss up to 77% of scotomas detectable through more sophisticated testing methods, highlighting the importance of comprehensive eye examinations.
The phenomenon of perceptual completion represents one of the grid’s most significant limitations, where the brain unconsciously fills in missing visual information, masking the presence of actual scotomas. This neurological adaptation mechanism, while beneficial for daily visual function, can prevent patients from recognising significant retinal pathology during Amsler grid testing. Additionally, the grid’s reliance on patient subjectivity introduces variability in reporting and interpretation that can affect diagnostic accuracy.
Fixation instability presents another challenge, particularly in patients with existing central vision impairment. When the foveal region is compromised, maintaining steady fixation on the central dot becomes difficult, leading to inconsistent testing results and potential false-negative findings. Furthermore, the grid’s limited dynamic range cannot detect subtle contrast sensitivity changes that may precede overt structural abnormalities in conditions such as early age-related macular degeneration.
Environmental factors significantly influence test reliability, including ambient lighting conditions, grid contrast, and viewing distance consistency. Variations in these parameters can alter test sensitivity and specificity, emphasising the need for standardised testing protocols. Patient education regarding proper testing technique proves crucial for obtaining meaningful results and ensuring that concerning changes receive appropriate clinical attention.
Understanding the limitations of Amsler grid testing helps both patients and clinicians appreciate when additional diagnostic evaluation is necessary and prevents over-reliance on this screening tool for comprehensive macular assessment.
Advanced macular function testing beyond traditional amsler grids
Modern ophthalmology has developed sophisticated alternatives and supplements to traditional Amsler grid testing that address many of its inherent limitations. These advanced assessment methods provide enhanced sensitivity for detecting subtle macular pathology and offer more precise characterisation of visual field defects.
Microperimetry represents a significant advancement in macular function testing, combining high-resolution retinal imaging with precise visual field assessment. This technology enables clinicians to correlate specific anatomical abnormalities with functional deficits, providing unprecedented insight into structure-function relationships in macular disease. Unlike static Amsler grid testing, microperimetry tracks eye movements and automatically adjusts stimulus presentation, ensuring accurate localisation of visual field defects even in patients with unstable fixation.
The preferential hyperacuity perimeter (PHP) addresses several Amsler grid limitations through sophisticated distortion detection algorithms and standardised stimulus presentation. This automated testing system presents dotted lines rather than continuous grids, reducing the influence of perceptual completion and increasing sensitivity for detecting metamorphopsia . Clinical studies demonstrate
that PHP technology demonstrates superior sensitivity compared to traditional Amsler grids, particularly for detecting early choroidal neovascularisation in age-related macular degeneration.
Shape discrimination hyperacuity testing offers another sophisticated approach to macular function assessment, utilising the eye’s remarkable ability to detect minute spatial distortions. This technique presents carefully controlled geometric patterns and measures the threshold for detecting shape alterations, providing quantitative assessments of macular function that far exceed the sensitivity of traditional grid testing. Research indicates that shape discrimination testing can detect functional abnormalities months before they become apparent on conventional Amsler grids.
Multifocal electroretinography (mfERG) provides objective assessment of macular function through electrical response measurements from different retinal regions. Unlike subjective testing methods, mfERG generates quantifiable data about photoreceptor and bipolar cell function across the central retina. This technology proves particularly valuable for monitoring disease progression and treatment response in conditions such as diabetic macular oedema and hydroxychloroquine retinal toxicity, where subjective symptoms may lag behind objective functional changes.
Optical coherence tomography angiography (OCTA) represents a revolutionary advancement in macular assessment, providing detailed visualisation of retinal and choroidal vasculature without invasive contrast injection. This technology enables clinicians to detect subtle vascular abnormalities associated with early neovascularisation, complement Amsler grid findings with objective anatomical data, and monitor treatment response in real-time. The correlation between OCTA findings and metamorphopsia symptoms helps validate patient-reported visual disturbances and guide clinical decision-making.
Clinical interpretation and patient education strategies
Effective clinical interpretation of Amsler grid results requires systematic evaluation protocols that consider patient-specific factors, testing conditions, and temporal changes in visual function. Healthcare professionals must distinguish between significant pathological findings and normal variations that occur with advancing age, refractive errors, or testing inconsistencies. The integration of grid testing results with comprehensive ophthalmological examination findings, including dilated fundoscopy, optical coherence tomography, and fluorescein angiography when indicated, provides the foundation for accurate diagnosis and appropriate treatment planning.
Patient education represents a critical component of successful Amsler grid implementation, encompassing proper testing technique instruction, realistic expectation setting, and clear communication about when to seek urgent medical attention. Many patients require repeated demonstrations to master the monocular testing protocol and understand the significance of maintaining consistent viewing distances and lighting conditions. Educational materials should emphasise that grid testing serves as a screening tool rather than a definitive diagnostic method, helping patients understand the importance of regular professional eye examinations even when home testing results appear normal.
The psychological impact of positive Amsler grid findings requires sensitive handling, as patients often experience significant anxiety upon discovering visual distortions. Healthcare providers must balance the urgency of prompt evaluation with reassurance that many macular conditions respond well to treatment when detected early. Clear explanation of the relationship between grid abnormalities and specific retinal pathologies helps patients understand their condition and participate actively in treatment decisions. This educational approach proves particularly important for patients with dry age-related macular degeneration who require long-term monitoring for conversion to the wet form of the disease.
Documentation strategies for Amsler grid findings should include detailed descriptions of distortion patterns, affected grid locations, and temporal changes in symptoms. Many clinicians provide patients with blank grid copies for marking abnormal areas, creating valuable records for tracking disease progression and treatment response. Digital photography of marked grids or smartphone applications with distortion mapping capabilities offer modern alternatives for maintaining accurate documentation. These records prove invaluable during follow-up appointments and enable clinicians to detect subtle changes that might otherwise escape notice.
The integration of Amsler grid testing into comprehensive eye care protocols requires consideration of patient-specific risk factors, including age, family history, systemic health conditions, and previous ocular pathology. High-risk individuals, such as those with large drusen or pigmentary changes, may benefit from daily grid testing combined with more frequent professional monitoring. Conversely, low-risk patients might adequately maintain their macular health through weekly testing and annual comprehensive eye examinations. This risk-stratified approach optimises healthcare resources while ensuring appropriate surveillance for vision-threatening conditions.
Quality assurance measures for Amsler grid testing encompass standardisation of testing materials, environmental conditions, and patient instruction protocols. Healthcare facilities should maintain consistent grid designs, lighting conditions, and viewing distance measurements to ensure reproducible results across different testing sessions and healthcare providers. Regular validation of digital testing platforms and smartphone applications helps maintain accuracy and reliability of modern grid testing methods. These quality measures contribute to improved diagnostic accuracy and enhanced patient confidence in the testing process.
The future of macular function assessment lies in combining the simplicity and accessibility of Amsler grid testing with advanced imaging technologies and artificial intelligence algorithms that can detect subtle changes in visual function before they become clinically apparent through traditional methods.